Making sure all at-risk children can access the vaccine is proving to be the key to a steeply falling prevalence of the chronic infection. From Gavi, the Vaccine Alliance.
by Hudson Kuteesa
First published June 16, 2025 by Gavi, the Vaccine Alliance

Two years ago, Clementine*, 32, visited the University Teaching Hospital of Kigali (CHUK). She was two-and-a-half months pregnant, and hadn’t planned to visit the health facility so soon. However, her husband had been recently diagnosed with hepatitis B, and she was concerned.
“I was feeling fine and had no symptoms, but when they tested me, I turned out to be positive. They checked my viral load and found it was very low, so I didn’t need to start medication at that time,” she recalls.
The medics at the hospital continued to follow up on her. When her baby was born six and a half months later, they immediately administered the hepatitis B vaccine to the newborn.
“The gynaecologist who was monitoring me knew that I was hepatitis B positive. After my caesarean section, she spoke with the paediatrician, and he gave the baby the vaccine,” she says.
There’s no cure for hepatitis B, a viral infection that can cause major liver damage, so prevention – with testing, treatment and vaccination – is at the forefront of Rwanda’s fight against the disease. Clementine is one of many people who have benefited: Rwanda has reduced the estimated prevalence of chronic hepatitis B from 3% in 2015, to 0.25% in 2024.
Protecting the next generation
According to the World Health Organization (WHO), an estimated 254 million people worldwide were living with chronic hepatitis B infection in 2022, with 1.2 million new infections every year. The WHO also says that in 2022 alone, hepatitis B resulted in an estimated 1.1 million deaths, mostly from cirrhosis and hepatocellular carcinoma (primary liver cancer).
Today, mothers themselves are asking to be tested for HBV when they visit health centres. The number of children being vaccinated has grown.
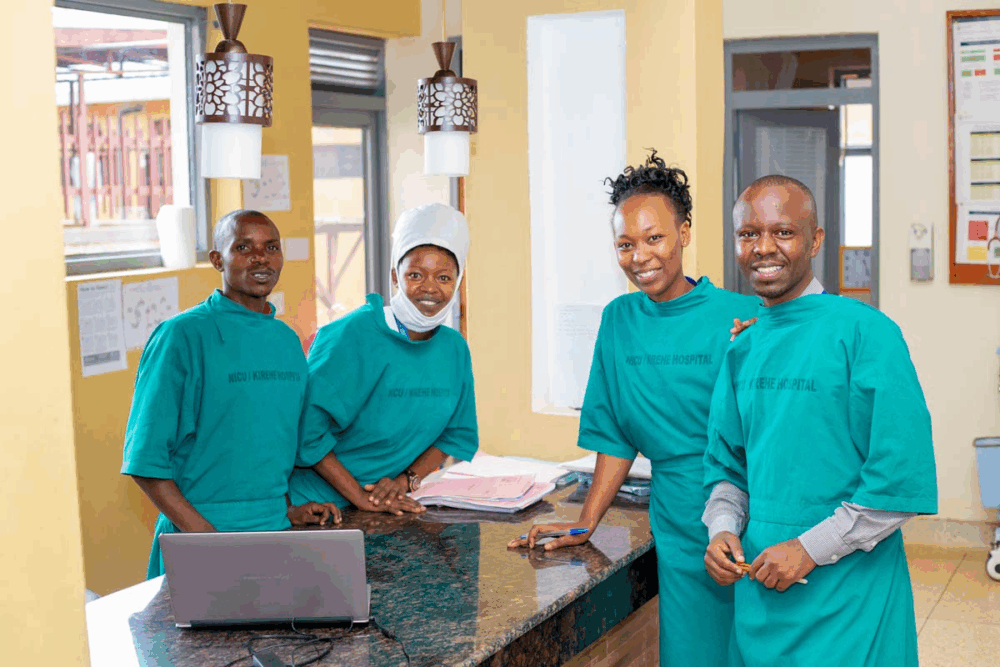
– Antoinette Dusabe, Maternity Nurse, Mibilizi Hospital
Dr Jean Damascene Makuza, a medical doctor, PhD student, and researcher specialising in hepatitis, told VaccinesWork that the most serious form of hepatitis B transmission is from mother to child because children’s immune systems cannot easily eliminate the virus.
“Children are more likely to develop chronic hepatitis B after infection. The key to prevention is timely vaccination, which stops mother-to-child transmission,” he says.
Clementine’s daughter is living proof. Today, she is one and a half years old, strong and healthy.
“I took her for all the routine vaccinations. She completed them all,” she says, pointing out that she has not for once taken the baby to a health centre for medical attention, since she has not suffered from any sickness, save for colds.
According to national guidelines, all pregnant women should be routinely screened for hepatitis B at their first antenatal visit and again at delivery. Those who test positive are followed up to assess if they need treatment, and the vaccine is administered to their newborns to prevent mother-to-child transmission. Routine vaccination activities are carried out across the country, including in places as remote as Rusizi, a far-west district that is more than 200 kilometres from Kigali.
Antoinette Dusabe, a maternity nurse at Mibilizi Hospital, one of two district hospitals in Rusizi district, says that pregnant women are becoming more and more aware of hepatitis B prevention. “Today, mothers themselves are asking to be tested for HBV when they visit health centres. The number of children being vaccinated has grown,” she noted.
The growing awareness of the disease in communities is partly due to sensitisation exercises by community health workers (CHWs), who have been a key part of Rwanda’s frontline workforce in tackling public health challenges over the past two decades.
The CHW’s roles include sensitising parents about the importance of vaccines, following up on children’s immunisation schedules, as well as providing nutritional advice.
7 million people vaccinated
Dr Hassan Sibomana, Director of Vaccination Programmes Unit at the Rwanda Biomedical Centre (RBC), says that since mother-to-child transmission during birth is the most common route of infection with hepatitis B – a “serious disease” in his terms – Rwanda, in collaboration with partners, is continuing to press forward to make sure every child at risk is protected.
General infant immunisation against HBV using the pentavalent vaccine has been in place since 2002 in Rwanda, and the national coverage reached 99% in 2020, according to the Rwanda Demographic Health Survey (DHS) 2019–2020.
RBC’s 2024 annual report on HIV, STIs and viral hepatitis, showed that from July 2023 to June 2024, 329,891 babies out of a total of 363,839 who were born in that period were given the pentavalent vaccine third dose, representing a coverage of 91%. More than 7 million people, including infants and adults, have benefited from vaccination programme, according to the report.
The birth dose is an additional and crucial protective measure against viral transmission from the mother. Going forward, Dr Sibomana says RBC is planning to roll out a programme that will give the hepatitis B vaccine birth dose to all newborns, irrespective of whether they are born to mothers who know they are infected or not.
Besides infant vaccination, Rwanda has a programme targeting adults born before 2002, the year during which the pentavalent vaccine was introduced in the country’s routine infant immunisation schedule.
This article was originally published on
VaccinesWork
Related Articles
Maldives Eliminates Mother-to-Child Transmission of HIV, Syphilis and Hepatitis B
The WHO has validated the Maldives as the first country in the world to achieve “triple elimination,” ensuring a healthier start for every child born in the country.

Hope Through Action: A Surgeon’s Mission to End Hepatitis B
Pioneering surgeon Dr. Samuel So founded Stanford’s Asian Liver Center to address high hepatitis B rates in Asian American communities. Through innovative outreach, advocacy, and policy reform, his work is transforming how America addresses this often-overlooked but deadly disease.
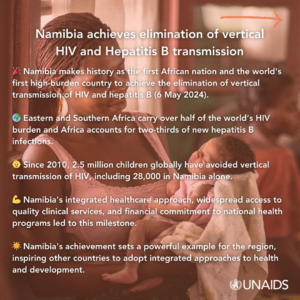
Namibia Achieves Milestone in Reducing Mother-to-Child HIV and Hepatitis B Transmission
The WHO has recognized Namibia’s significant progress in reducing mother-to-child transmission of HIV and hepatitis B, setting an example for other African countries to follow.
