A nationwide study suggests infections with human papillomavirus (HPV) types 16 and 18 have been virtually eliminated since vaccination began in 2008 – protecting even unvaccinated women.
by Linda Geddes
First published September 2, 2025 by Gavi, the Vaccine Alliance

Denmark has effectively eliminated infections with the two biggest cancer-causing strains of human papillomavirus (HPV) since the vaccine was introduced in 2008, data suggests.
The research, published in Eurosurveillance, could have implications for how vaccinated populations are screened in the coming years – particularly as people increasingly receive vaccines that protect against multiple high-risk types of HPV virus.
Before vaccination, the prevalence of HPV16/18 was between 15 and 17%, which has decreased in vaccinated women to less than one percent by 2021.
– Researchers, Eurosurveillance
Deadly cancer
After breast cancer, cervical cancer is the most common type of cancer among women aged 15 to 44 years in Europe, and human papillomavirus (HPV) is the leading cause.
At least 14 high-risk types of the virus have been identified, and before Denmark introduced the HPV vaccine in 2008, HPV types 16 and 18 accounted for around three quarters (74%) of cervical cancers in the country.
Initially, girls were offered a vaccine that protected against four types of HPV: 16, 18, plus the lower risk types 6 and 11. However, since 2017, Danish girls have been offered a vaccine that protects against nine types of HPV – including those accounting for approximately 90% of cervical cancers.
To better understand the impact that these vaccination programmes have had on HPV prevalence as vaccinated girls reach cervical screening age (23 to 64 years in Denmark), Dr Mette Hartmann Nonboe at Zealand University Hospital in Nykøbing Falster and colleagues analysed up to three consecutive cervical cell samples collected from Danish women between 2017 and 2024, when they were 22 to 30 years of age.
“In 2017, one of the first birth cohorts of women in Denmark who were HPV-vaccinated as teenage girls in 2008 reached the screening age of 23 years,” Nonboe explained.
“Compared with previous generations, these women are expected to have a considerably lower risk of cervical cancer, and it is pertinent to assess [their] future need for screening.”
High-risk HPV elimination
The research found that infection with the high-risk HPV types (HPV16/18) covered by the vaccine has been almost eliminated.
“Before vaccination, the prevalence of HPV16/18 was between 15 and 17%, which has decreased in vaccinated women to less than one percent by 2021,” the researchers said.
In addition, prevalence of HPV types 16 and 18 in women who had not been vaccinated against HPV was five percent. This strongly suggests that the vaccine has reduced the circulation of these HPV types in general population, to the extent that even unvaccinated women are now less likely to be infected with them – so called “population immunity” – the researchers said.
In 2017, one of the first birth cohorts of women in Denmark who were HPV-vaccinated as teenage girls in 2008 reached the screening age of 23 years. Compared with previous generations, these women are expected to have a considerably lower risk of cervical cancer.
– Mette Hartmann Nonboe, Researcher, Eurosurveillance
Despite this good news, roughly one third of women screened during the study period still had infection with high-risk HPV types not covered by the original vaccines – and new infections with these types were more frequent among vaccinated women, compared to unvaccinated ones.
This is expected to fall once girls who received the more recent ‘nine-valent’ vaccine reach screening age. At this point, the screening guidelines should potentially be reconsidered, Nonboe and colleagues said.
This article was originally published on
VaccinesWork
Related Articles

In Zimbabwe, Youth Champions Are Taking the Fight to Cervical Cancer
Younger voices are better heard by their peers, say health workers campaigning for improved HPV vaccine uptake. From Gavi, the Vaccine Alliance.
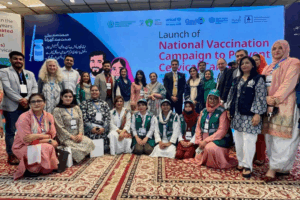
A Turning Point for Women’s Health in Pakistan
Starting in September 2025, the nation’s daughters will be shielded from a brutal and preventable disease — cervical cancer, from HPV — and we’re glad to play our part in the campaign. Story by Gavi, the Vaccine Alliance.
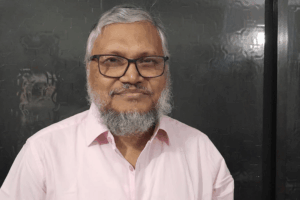
The ‘Pink Man’ of Bangladesh and His Battle Against Female Cancers
Breast and cervical cancers account for nearly a third of all cancer diagnoses in Bangladeshi women – and mortality rates have been way higher than Dr Habibullah Talukder Ruskin is willing to accept. From Gavi, the Vaccine Alliance.
