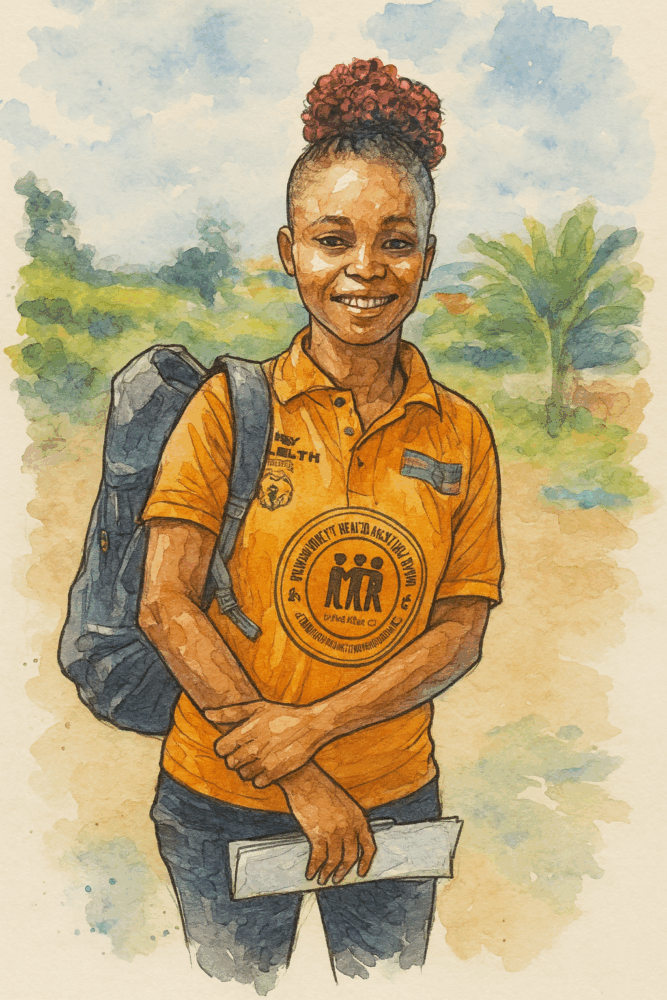
In the rainforests of Grand Bassa County, Liberia, community health worker Victoria Karpay knows every family in her village of Taye Town. When a child develops a fever in the middle of the night, parents don’t face the agonizing choice of attempting a two-day journey through dense forest and across rivers to reach the nearest clinic. Instead, they walk to Victoria’s home, where she can diagnose and treat malaria within minutes.
“Since I started working as a community health worker, I have experienced no child death in my community,” Victoria says with quiet pride. Her words carry weight in a country where, not long ago, preventable diseases claimed thousands of young lives each year.
Victoria is one of nearly 5,000 community health workers deployed across Liberia as part of a revolutionary healthcare model pioneered by Last Mile Health, an organization that has transformed how the world thinks about delivering care to remote communities.
Born from Crisis, Built on Hope

The story of Last Mile Health begins with a nine-year-old boy fleeing civil war. In 1989, as violence engulfed Liberia, Raj Panjabi and his family escaped on a rescue cargo plane to Sierra Leone, eventually finding refuge in the United States. The son of Indian immigrants who had made their life in West Africa, Panjabi carried with him both the trauma of displacement and a deep connection to the country he’d been forced to leave behind.
Sixteen years later, Panjabi returned to Liberia as a 24-year-old medical student, determined to help rebuild the nation’s shattered healthcare system. What he found was devastating: a country with fewer than 50 doctors serving 4 million people, where 1.2 million citizens lived more than an hour’s walk from the nearest health facility. In remote villages, mothers watched their children die from malaria, diarrhea, and pneumonia—diseases that could be treated with basic medications costing pennies.
In 2007, at his wedding to Amisha Raja, instead of traditional gifts, the couple asked guests to donate to a vision: bringing healthcare directly to Liberia’s most isolated communities. They raised $6,000. With this modest sum and partnership from Liberian civil war survivors and American health workers, Last Mile Health was born.
The Community Health Worker Model: Professional, Paid, and Powerful

What makes Last Mile Health’s approach revolutionary isn’t just the deployment of community health workers—it’s their insistence that these workers be treated as healthcare professionals. In a field where 60% of community health programs in East Africa rely on unpaid volunteers, Last Mile Health championed a different model: workers who are skilled, salaried, supervised, and supplied.
The organization’s community health assistants undergo months of rigorous training, learning to diagnose and treat the leading causes of childhood mortality: malaria, diarrhea, and acute respiratory infections. They’re equipped with rapid diagnostic tests, essential medications, and digital tools for tracking patient data. Crucially, they’re supported by nurse supervisors who conduct regular field visits, ensuring quality care and providing ongoing mentorship.
In Liberia, these workers earn $70 per month—a modest sum by Western standards but a living wage that recognizes their essential role in the healthcare system. This professionalization has been key to the program’s success and sustainability.
From Pilot to National Scale
Last Mile Health’s journey from a small pilot program to a national healthcare transformation reads like a blueprint for systemic change. In 2012, they partnered with Liberia’s Ministry of Health to launch a community health worker program in Konobo District, one of the country’s poorest and most remote regions. Within a year, they achieved 100% coverage of the district, with skilled birth attendance rising from 55% to 84%.
The results caught the attention of the Ministry of Health, which invited Last Mile Health to help design and launch the National Community Health Assistant Program in 2016. This wasn’t just another NGO project—it was a fundamental reimagining of how the country delivered healthcare.
The timing proved critical. When the program launched, Liberia was still recovering from the 2014-2016 Ebola epidemic that had exposed the deadly consequences of weak health systems. The epidemic had claimed over 4,800 lives in Liberia alone, but it also demonstrated something powerful: in communities where Last Mile Health had trained workers, routine health services continued uninterrupted throughout the crisis.
The Road to Full Scale
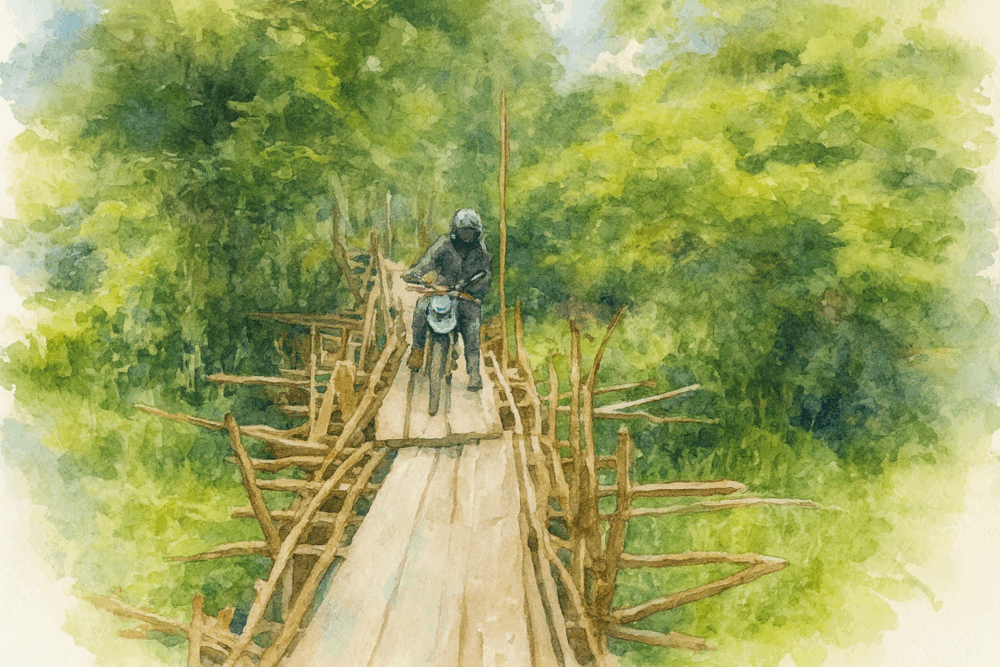
Building a national healthcare program in a country with limited infrastructure required navigating countless challenges. Roads that become impassable during rainy season. Communities accessible only by canoe. A healthcare workforce where only 17% of paid community health workers were women, despite evidence showing female health workers often achieve better maternal and child health outcomes.
Last Mile Health and the Ministry of Health tackled these challenges systematically. They developed new training curricula optimized for low-literacy learners. They pioneered digital tools that could function offline, allowing workers to collect and sync data even in areas without electricity or internet. They implemented gender-inclusive recruitment strategies, working to increase female participation in the workforce.
The partnership with the government proved essential. As Dr. Raj Panjabi noted, “The only way our vision of a health worker within reach of everyone everywhere is possible is through national community health programs.” This wasn’t about creating a parallel system—it was about strengthening and transforming the existing one.
By June 2024, Liberia achieved what many thought impossible: full scale of the National Community Health Assistant Program. Every remote community in the country now has access to a trained, equipped community health worker. It’s a remarkable achievement that positions Liberia as a global leader in universal health coverage.
Measuring Impact, Saving Lives
The numbers tell a powerful story. Since 2016, Liberia’s community health workers have:
- Delivered over 1.5 million treatments to children under five
- Conducted more than 14 million home visits
- Treated 45% of all malaria cases in children under five in rural areas
- Achieved zero maternal deaths and zero child deaths in many previously underserved communities
Research published in the American Journal of Public Health demonstrated that in areas with the program, the proportion of children receiving care from a qualified provider increased by over 60% compared to areas without coverage. These aren’t just statistics—they represent thousands of children who are alive today because care reached them in time.
When Liberia launched its first malaria vaccine campaign in 2024, community health workers were integral to the rollout, conducting community education, tracking children to ensure they received all four doses, and serving as the trusted bridge between modern medicine and traditional communities.
Beyond Liberia: A Model for the World
Last Mile Health’s success in Liberia has attracted international attention and investment. In 2019, Co-Impact, a collaborative philanthropy initiative, partnered with the organization and the Global Fund to invest $20 million in scaling and sustaining Liberia’s community health system. The partnership serves as a model for how governments, NGOs, and philanthropic organizations can work together to drive systemic change.
The organization has expanded its work to Ethiopia, Malawi, and Sierra Leone, adapting its model to different contexts while maintaining core principles. In Ethiopia, they’re using digital technology to train 40,000 existing community health workers. In Malawi, they’re strengthening the quality of care through improved supervision and data systems.
Across all four countries, Last Mile Health and its government partners now support more than 16,000 community and frontline health workers, serving over 19 million people. Their Community Health Academy, launched with the $1 million TED Prize awarded to Panjabi in 2017, has trained tens of thousands of health workers from nearly 200 countries through digital courses.
The Human Face of Healthcare
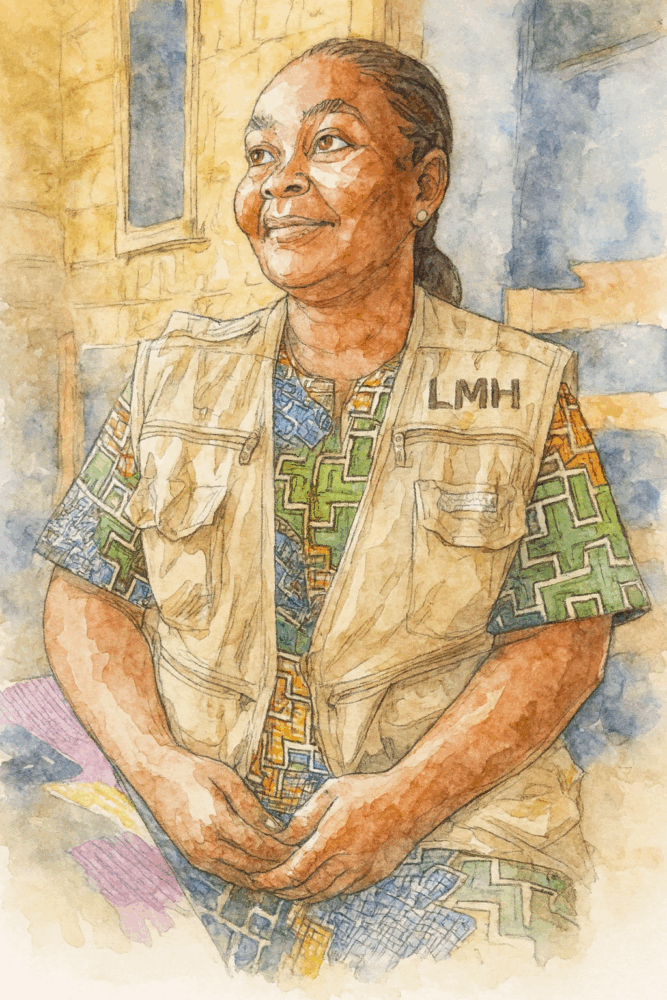
Behind every statistic is a story like that of Laura Gbee, a community health worker in Grand Bassa County, or Marie Gboto, who brought her son Samuel to Laura when he woke dangerously ill with a high fever. In the past, Marie would have faced an impossible journey to reach care. Now, Laura could diagnose and treat Samuel’s malaria immediately, likely saving his life.
These workers aren’t just delivering medications—they’re transforming how communities understand and engage with healthcare. They educate families about disease prevention, connect pregnant women with prenatal care, ensure children receive their immunizations, and serve as the early warning system for disease outbreaks.
For many community health workers, the role represents more than a job. Victoria Karpay describes the respect, trust, and relationships she’s built with her community. Some, like her, aspire to continue their education and become nurses, creating a pipeline of healthcare professionals drawn from and committed to serving rural communities.
Looking Forward: Healthcare as a Human Right
As climate change drives new health challenges and future pandemic threats loom, Last Mile Health’s model offers crucial lessons. Community health workers aren’t just stopgaps for physician shortages—they’re essential components of resilient health systems capable of responding to crises while maintaining routine care.
The organization continues to advocate globally for professional community health workforces, contributing to the World Health Organization’s first-ever community health worker guidelines and demonstrating that with proper investment, universal health coverage is achievable even in the world’s poorest countries.
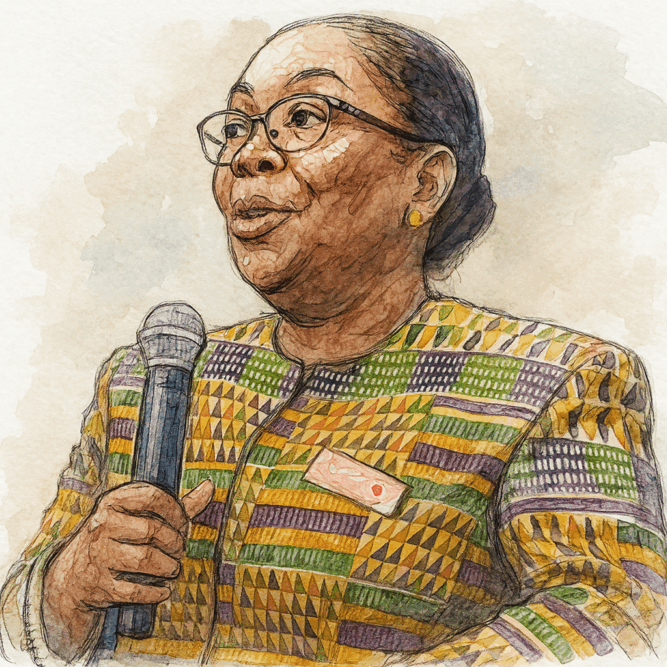
Dr. Bernice Dahn, Liberia’s former Minister of Health, captured the program’s significance: “Liberia has made great progress building a government-led and unified national community health worker program that is rooted in quality. This program demonstrates what’s possible when governments invest in community health workforces to advance universal health coverage.”
The Distance That Remains

While Last Mile Health has achieved remarkable success, the global challenge remains staggering. The World Health Organization estimates that half the world’s population still lacks access to essential health services. Nearly 9 million people die annually from preventable causes due to lack of healthcare access.
Last Mile Health’s vision—”Until no patient is out of reach”—acknowledges both how far we’ve come and how far we still need to go. But in communities across Liberia, Ethiopia, Malawi, and Sierra Leone, that vision is already a reality. Children who would have died from treatable diseases are growing up healthy. Mothers are surviving childbirth. Communities that were invisible to health systems are now connected to care.
As Raj Panjabi often quotes his father: “No condition is permanent.” Not poverty, not isolation, not lack of healthcare access. With the right investment in community health workers, even the most remote communities can be brought within reach of quality healthcare.
The model that began with $6000 in wedding gifts has become a blueprint for achieving universal health coverage in some of the world’s most challenging settings. It’s proof that with vision, partnership, and respect for community health workers as professionals, we can bridge the distance between illness and care, between isolation and connection, between despair and hope.
For the families in villages like Taye Town, that bridge has a name and a face—someone like Victoria Karpay, who ensures that no fever goes untreated, no mother delivers alone, and no community remains beyond the reach of healthcare.
Read more about Victoria Karpay and her work for Last Mile Health: “My community has been uplifted”: A profile of community health worker Victoria Karpay
Watch this video from Last Mile Health from January 2025:
Watch this Ted Talk by Dr. Raj Panjabi from 2017:
Related Articles

Affordable Microscope Speeds Up Malaria Diagnosis with AI
The Octopi microscope autonomously analyzes blood samples in minutes, detecting malaria-infected cells among millions. Its creators hope it will accelerate the fight against malaria. From Stanford Report.

Risky, Tiring and Worth it: the Volunteer Vaccinators Protecting Children in Rural Liberia
Vaccinators Harrison Moore and Jerry Karn ford rivers, navigate potholed, mud-slick roads, and do it all without pay. From Gavi, the Vaccine Alliance.
Last Mile Health: Bringing Healthcare to the Most Remote Communities
Last Mile Health transforms healthcare delivery in remote communities by training and paying local health workers, ensuring no patient is out of reach in Liberia, Ethiopia, Malawi, and Sierra Leone.
