A physician who confronted Marburg in Rwanda and, previously, COVID-19 in New York, demonstrated what’s possible with bravery and supportive systems.
Dr. Tsion Firew has spent her career responding to crises, from war zones to pandemics. But nothing prepared her for the personal cost of Rwanda’s first Marburg outbreak.
As Chair of Emergency Medicine at Africa Health Sciences University in Rwanda, Firew found herself at the center of a deadly outbreak in September 2024, watching colleagues fall ill and die from a virus that has previously killed nine out of ten patients. She sent her young children away to Ethiopia, updated her life insurance, and continued treating patients even as hallucinations from exhaustion haunted her empty home at night.
The outbreak began with a 27-year-old miner who likely contracted the virus from a bat. Within days, Firew witnessed the rapid deterioration of a young nurse she’d worked alongside. “It was quite scary, because you had no idea what you were dealing with,” she told NPR’s Goats and Soda, one year after the outbreak.
When the nurse died, leaving behind a partner and toddler, the reality set in. Firew had hugged a colleague in a hospital hallway who then developed symptoms. Her husband was stranded in Atlanta after Hurricane Helene. Alone and terrified she might have exposed her 1- and 3-year-old children, she made the wrenching decision to send them to family out of the country. Days later, her son developed a fever in Ethiopia, and Firew briefly bought—then canceled—a ticket to be with him.
Firew’s resolve came in part from her experience during the covid pandemic, when she worked at Columbia University Medical Center in New York City. In a 2020 Guardian interview, she described the devastation at Columbia’s smaller hospital near the Bronx, where “people were dying in ambulances while waiting for care” and the emergency department was overwhelmed with patients needing oxygen. She and her husband both contracted covid, and she recalled the stark fear: “Walking from my bed to the kitchen would make my heart race; I often wondered: is this when I drop dead like my patient the other day?”
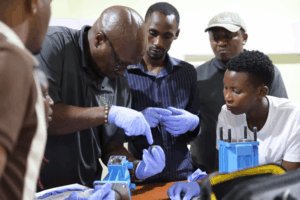
In Rwanda, she found a government that acted swiftly, establishing testing and isolation wards immediately, launching a vaccine trial within ten days, and ensuring adequate supplies of protective equipment.
Firew proposed an unprecedented approach: starting exposed healthcare workers on the experimental drug remdesivir prophylactically, before they developed symptoms. The idea was approved and implemented within 48 hours, treating over 150 healthcare workers. She also helped administer the first-ever monoclonal antibody infusion to a Marburg patient, including the colleague who had hugged her in the hallway, who survived.
Rwanda’s outbreak ended in December 2024 with a historic 23% fatality rate, the lowest ever recorded for Marburg. Of 66 patients, 15 died; more than three-quarters were healthcare workers. After six weeks apart, Firew’s family finally reunited at the Kigali airport.
She wishes the world could see Rwanda’s response as proof of what belief in science can achieve: “This work, this effort did not go to waste. It is not futile.”
This summary is based on the following articles:
- A bold doctor sent her kids away and helped beat one of the world’s deadliest viruses, by Gabrielle Emanuel for NPR’s Goats and Soda
- ‘Is this when I drop dead?’: two doctors on their time at the Covid frontline, by Tsion Firew and Cedric Dark for The Guardian
Listen to the podcast from NPR’s Goats and Soda:
Related Articles

Rwanda is Knocking on Every Door in a Bid to End Cervical Cancer
Getting over the cervical cancer elimination line means both vaccinating girls and screening women. Rwanda’s corps of volunteer health workers are going door to door to get it done. From Gavi, the Vaccine Alliance.
Biomedical Engineering Training Center Takes Off
Build Health International’s new training center in Kigali, Rwanda, is teaching biomedical engineers and technicians how to keep oxygen systems and life-saving medical equipment running in hospitals across East Africa.

A Legacy of Health Equity: Agnes Binagwaho Receives Cameron Award
The Cameron Award, from the RCSI School for Population Health, honors Professor Agnes Binagwaho for her transformative work rebuilding Rwanda’s health system and advancing equitable healthcare access in resource-limited settings worldwide.