A mobile health program run by Northwell Health and the Long Island Coalition for the Homeless is reaching patients who might otherwise never see a doctor, and helping some find their way off the streets.
In a commuter parking lot behind a McDonald’s, in a space tucked beside a Popeyes in Brentwood, in the shadow of the Long Island Expressway’s relentless traffic, a medical team is conducting house calls for people who have no houses.
Northwell Health’s Street Medicine program, a collaboration with the nonprofit Long Island Coalition for the Homeless, dispatches nurses and clinicians to reach homeless Long Islanders wherever they are—in cars, in tents, in the overlooked corners of one of America’s wealthiest suburbs. About 10,000 Long Islanders experience homelessness each year, and many face chronic illness, mental health challenges, and substance use disorders without access to consistent medical care.
“People having a tough time of it should not be shut out from access to even the most basic health needs,” Dr. Debbie Salas-Lopez, executive vice president of Northwell’s Institute for Community Health and Wellness, told Northwell Health. “Being heard can be therapeutic. Getting help can be life-changing.”
The program, which launched in mid-2024, has logged more than 3,800 miles traveling across Nassau and Suffolk counties, from Hempstead to Wading River and out to the East End. The team has served 93 patients through more than 200 encounters, providing primary care services, prescriptions, referrals to specialists, and, for 11 patients so far, help finding stable housing.
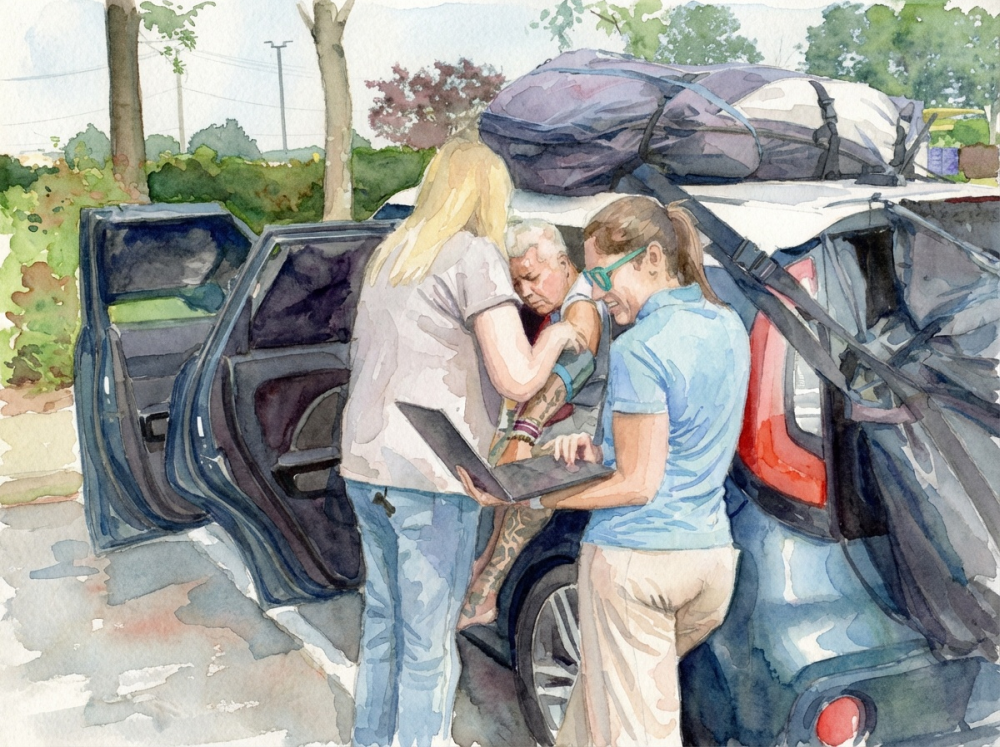
For Virginia Collins, 66, the team arrived at a moment of crisis. Collins had suffered a stroke in Florida before driving back to New York, where she found herself living in her car in a central Suffolk parking lot, unable to secure housing that would allow her to keep her dogs. When the Street Medicine team found her, she was experiencing headaches and hearing loss.
“My days are numbered,” Collins told Northwell Health last August. “I originally thought I was going to die here in this car. There was no hope. Meeting people who care is great.”
The medical volunteers arranged a neurology appointment—the kind of specialist referral that can seem impossibly out of reach for someone without an address or reliable transportation.
For Bryan, 50, and his partner Jenny, 43, the program has been similarly critical. The couple has been homeless for three years, sleeping in a tent through Long Island winters. Bryan nearly died multiple times from blood clots and pulmonary embolism before connecting with the Street Medicine team.
“They are saving lives,” Bryan told ABC 7 NY. “That’s my angel crew right there.”
The obstacles to treating homeless patients extend well beyond logistics. Many are managing multiple chronic conditions while struggling to secure food and shelter. “When you’re fighting for your next meal, it could be difficult to prioritize getting to the doctor,” Dylan Schwarz of the Long Island Coalition for the Homeless told ABC 7 NY.
The Long Island Coalition for the Homeless, founded in 1985 as a grassroots advocacy effort, is the lead organization addressing homelessness across Nassau and Suffolk counties. Now in its 40th year, the organization provides housing-focused case management, operates a helpline for navigating resources, and coordinates referrals to homeless-dedicated housing programs.
The program’s clinicians understand that meaningful care requires more than medical intervention. “What we have learned is that dignity and being treated with respect is so important,” Dr. Salas-Lopez said.
The ultimate goal is not just treatment but stability. The Coalition for the Homeless canvasses the region to identify people with healthcare needs, and the Street Medicine team helps patients navigate the bureaucratic requirements for housing: physicals, psychiatric evaluations, and disability documentation. So far, 35 clients have received help with that process.
Richard Seibert, 65, is among those who have made it through. After meeting with the team outside the Freeport Memorial Library, he secured housing in Hempstead. “Once I settle in, then I can concentrate on real things—employment and working on getting a car,” he told Northwell Health. “I’m looking forward to getting back to a normal life.”
For Jenny and Bryan, that kind of stability remains out of reach. In December, they met with the medical team in icy rain outside the Brentwood Popeyes. It was another visit to monitor Bryan’s high blood pressure, and another effort by clinician Jennifer Stevens to persuade him to stay on his medication.
“I wish that I had more to give to my family,” Jenny said to ABC 7 NY. The couple has three children.
A home would improve their health outcomes. But for now, being seen, and being treated as people whose lives matter, offers something essential.
“Hope exists where they venture,” as Northwell put it, “because the medical volunteers bring tangible care and the prospect of more permanent fixes to persistent health problems.”
Watch the news story from ABC 7 NY:
This summary is based on the following stories:
- Northwell Street Medicine Team brings life-saving care straight to the homeless, by Stacey Sager for ABC 7 NY
- Northwell delivers house calls to homeless, Northwell Health
Related Articles

Street Outreach Brings Health Care to Detroit’s Unhoused
Nurse Stanley Stinson and dedicated volunteers deliver vital healthcare directly to Detroit’s unhoused, building trust and transforming lives with support from The Pfizer Foundation and Direct Relief.

From Bus to Lifeline: Kansas City’s Mobile Clinic Expands Amid Healthcare Crisis
Care Beyond the Boulevard delivers essential medical services to Kansas City’s homeless and uninsured communities, expanding from a volunteer-run mobile clinic to a vital healthcare provider filling gaps left by recent clinic closures.

Street Medicine’s New Frontier: Bringing Psychiatric Care to LA’s Homeless
Dr. Shayan Rab and the Los Angeles County Homeless Outreach & Mobile Engagement (HOME) program are revolutionizing mental health treatment by bringing psychiatric care directly to those living on the streets.


